News / Blog
Top 10 Tips for Using Tibial Interlocking Nail Effectively?
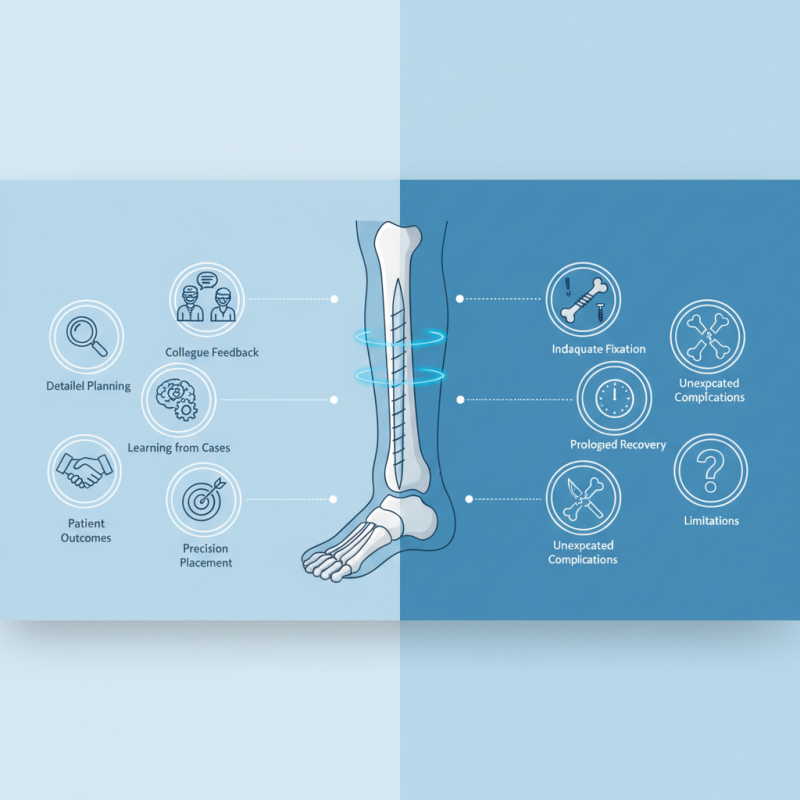
The Tibial Interlocking Nail is a vital tool in orthopedic surgery, used for stabilizing fractures in the tibia. Proper use of this device can significantly improve patient outcomes. However, mastering its application requires understanding both its benefits and limitations. Unexpected complications can arise if the technique is not executed correctly.
Surgeons must pay close attention during placement. Each step should be approached with precision. Common challenges include misalignment and inadequate fixation strength. These issues can lead to prolonged recovery times. It is crucial to reflect on previous cases and learn from mistakes.
Detailed planning is essential before surgery. Visualizing the procedure can help address potential pitfalls. Moreover, incorporating feedback from colleagues can enhance skills. The Tibial Interlocking Nail, while effective, demands careful consideration and ongoing practice. This balance of confidence and caution is key for successful outcomes.
Understanding the Basics of Tibial Interlocking Nail Anatomy and Function
The tibial interlocking nail is a vital tool in orthopedic surgery. Its design includes a long metal rod inserted into the tibia. This rod is locked in place with screws at each end. Understanding its anatomy is crucial for effective use. The nail often features a central canal, which minimizes bone removal and supports healing.
The interlocking mechanism provides stability for fractured bones. However, improper placement can lead to complications. It’s common to overlook the angle of insertion, which can affect alignment. Surgeons should carefully plan the entry point and trajectory. Attention to detail during this phase is essential for success.
Post-surgery, monitoring is key. Patients may experience discomfort that can interfere with recovery. It’s important to adjust rehabilitation strategies based on individual progress. Reflecting on surgical outcomes can enhance future practices. Understanding the anatomy and function of the tibial interlocking nail is a continuous learning process.
Preoperative Planning: Key Considerations for Successful Nail Insertion
Preoperative planning is crucial for successful tibial interlocking nail insertion. Surgeons must assess the patient's anatomy and injury type. X-rays help identify bone alignment and any fractures. It's important to consider the condition of the soft tissues as well. A thorough evaluation can help predict potential complications.
Surgeons should also determine the optimal entry point for the nail. It must align with the tibial canal. Misalignment can lead to difficulties during insertion. Additionally, establishing correct nail length is vital. Too short may compromise stability, while too long could damage surrounding structures.
Effective communication with the surgical team is essential. Discuss the procedure and expectations. Team members should understand their roles in managing instruments and monitoring the patient. Planning can often highlight gaps in knowledge or skills. Identifying these areas allows for focused training and improvement.
Step-by-Step Insertion Techniques for Tibial Interlocking Nail Use
Tibial interlocking nail insertion requires precision and careful technique. The first step involves proper positioning of the patient. The leg should be aligned in a neutral position. This allows easier access to the medullary canal. Proper imaging is essential. Ensure that the X-ray images are clear to guide the insertion.
Next, select the right size of the nail based on the patient's anatomy. This involves measuring the diameter and length accurately. Using improper sizes can lead to complications. After this, make a small incision at the knee region. This gives entry to the medullary canal. It's important to avoid excessive soft tissue damage during this step.
Drilling into the bone requires attention. Ensure that the drill bit is stable. Reassess your angle frequently. A poorly angled entry can cause misalignment issues later on. Once the nail is in place, lock it with screws. Pay attention to the tightening process. Over-tightening can lead to fractures in surrounding bone. Regularly reflect on your technique. Each insertion provides a learning opportunity for future procedures.
Top 10 Tips for Using Tibial Interlocking Nail Effectively
This chart illustrates the effectiveness of various techniques used for tibial interlocking nail insertion, measured by the percentage of successful operations in a clinical study.
Postoperative Care and Monitoring for Optimal Recovery Outcomes
Postoperative care is essential for optimal recovery after tibial interlocking nail surgery. Patients should monitor their surgical site for any signs of infection, such as redness or unusual swelling. Keeping the area clean is vital. Regular follow-ups with healthcare providers help track recovery progress.
For effective use of tibial interlocking nails, consider these tips. Perform gentle range-of-motion exercises as soon as the doctor allows. This helps maintain flexibility. Paying attention to pain levels during these exercises is crucial. If pain exceeds acceptable levels, it may be time to adjust the routine.
Nutrition plays a significant role in healing. A diet rich in proteins, vitamins, and minerals supports tissue repair. Consuming enough calcium and vitamin D promotes bone health, which can speed up recovery. Staying hydrated is also important. It’s easy to forget about fluids, but dehydration can delay healing.
Common Complications and How to Mitigate Risks During Procedure
Tibial interlocking nailing is a common orthopedic procedure. However, complications can arise during the process. According to a study published by the Journal of Orthopedic Trauma, 20% of patients experience complications, such as infection or malalignment. This emphasizes the importance of precise techniques and adherence to safety protocols.
Infection rates can reach 8.7% in some cases. Proper sterile techniques and the use of prophylactic antibiotics are crucial. Using imaging guidance can help ensure accurate nail placement. It reduces the risk of damaging surrounding tissues and minimizes malalignment. The challenge is achieving optimal alignment while avoiding intraoperative errors.
Surgeons must also address the risk of nonunion or malunion. Data suggests that 9% of patients may face these issues without careful monitoring. Regular follow-ups and imaging can help catch problems early. Some might overlook the importance of these follow-ups. This can lead to longer recovery times and additional surgeries. The goal is to improve patient outcomes by staying vigilant throughout the healing process.
